SPECIALIST AREAS

The treatments at The Oving Clinic can be organized in the form of specialist programmes that focus
on specific needs of groups of patients.

It is essential for any sports person to minimise the impact of sports injuries on the ability to participate and complete. The importance of keeping people fit during the recovery process is vital. Cross-training, relative rest and support of injured structures make this possible.
Our team at The Oving Clinic offers an extensive range of treatments to achieve this. We have a wealth of experience within the sports injuries field. Some or all of the following services can be selected depending on the individual’s needs. We liaise closely with all parties: the sports person, coach, manager and GP
DIAGNOSIs
We provide early diagnosis in order to facilitate a speedy recovery; and full Sports Science back up for further analysis provided by colleagues in Sportswise Eastbourne or London.
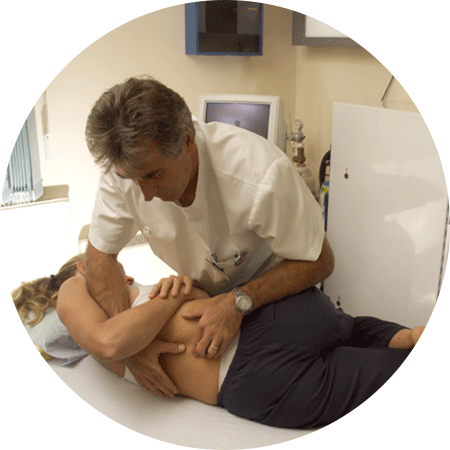
TREATMENT
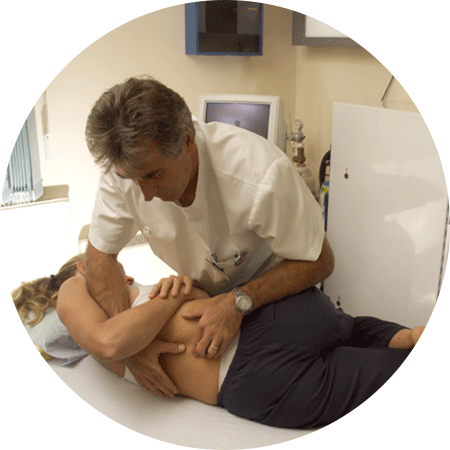
Treatment is carried out by Dr Tanner, who specialises in musculoskeletal and sports medicine, and our team of physiotherapists. This may include manual and assisted active mobilisation, injection techniques and electrotherapy.
PODIATRY
Where necessary, we offer podiatry involving assessment of gait, lower limb function, biomechanical analysis and design of
custom-made insoles.
REHABILITATION/PREVENTION
After the tissues have recovered enough to take the strain, we direct a graded return to pre-injury fitness through physiotherapy. A variety of techniques are used to mobilise and stabilise problem areas: these include manipulation, specific exercise, postural training and taping. Preventative measures such as adjustment of training programme, correction of faulty technique,advice on equipment and specific stretching and strengthening programmes are used.
OPTIMISING PERFORMANCE
This can be achieved by identifying musculoskeletal strengths and weaknesses; developing a personal programme; advice on nutrition; consultation with the coach; and full Sports Science back-up.
SPORTS AIDS
The most common reason for absenteeism from work is musculoskeletal pain. Our 12-point plan looks at how businesses can address this issue through analysis, ergonomics, treatment, fitness and stress management.
We have a wealth of experience in this area (British Gas, the Hampshire Police Force, Railtrack, IBM, Transco and South West Trains).
Our team of experienced and qualified practitioners offers an extensive selection of skills, treatments and therapies. This enables us to cross-refer and treat not only the physical aspects of the patient, but also the psychological and social.
Companies can choose some or all of the services in this programme. Patients are treated at our clinic or treatment rooms can be set up at the workplace either on a temporary or permanent basis. Qualified instructors can be provided to teach classes during the lunch hour or after work.
We liaise closely with all parties; the employee, the employer, physicians and other members of the Occupational Health Team including personnel and the employee’s GP.
12-POINT PLAN
1. Diagnosis of musculoskeletal problems with specialist back up.
2. Identifying any intrinsic or exrinsic factors that might influence the employee’s recovery.
3. Treatment for patients with particular or acute problems.
4. Low cost, high tech investigations and streamlined referrals to appropriate surgical specialists.
5. A pvhased return to work, or specific treatment that enables the employee to continue at work (i.e. with support and modified activities/work schedule).
6. Assessment of all/key employees for musculoskeletal risk factors.
7. Specific fitness programmes for high risk employees.
8. Advice on preventative measures and educating employees regarding their weaknesses in order to promote ‘self help’.
9. Advice on ergonomics (including statutory requirements).
10. Supply postural/musculoskeletal aids.
11. Stress management can be provided in light of the new legislation on stress-related disorders.
12. Preparation of medico-legal reports.

ASSESSMENT
A thorough assessment is given to clients wishing to embark on this programme which involves looking at areas such as cardiovascular and muscular endurance, strength, flexibility, speed, power, agility and coordination. A full medical history is also obtained.
PERSONAL PROGRAMMES
After analysing information gathered from the assessment, our team of physiotherapists will work with clients to devise a personal exercise programme.
NUTRITION
Nutrition plays an important part in the programme. A healthy, well balanced diet can help achieve fitness, a greater energy level, better complexion and positive attitude. We look at the individual’s eating habits and discuss how they could be improved.
RELAXATION
Allowing time for rest and relaxation is essential. We look at different methods of relaxation and help clients choose the most suitable one for them.
TRAINING
Once the individual training programme has been prepared, clients are encouraged to continue with the exercises at home or at the gym. Follow up appointments are held at the clinic after 6 weeks and programmes updated. For those who find it hard to exercise on their own, we can recommend a fully qualified personal trainer to visit the client’s home. Sessions may include jogging, step, aerobics, free weights, toning and stretching.
Good posture, correct breathing, digestion and co-ordinated activity of upper and lower limb movements are vital for spinal health. In order to achieve these we need stability, flexibility, strength and control. If you are in pain, one or more of these components is affected.
DIAGNOSIS
This is the first step and a full assessment of all factors is essential.
These include:
Posture and movement patterns.
Joint mobility.
Muscle weakness or tension.
Ligament strain or slackening.
Degenerative or osteoarthritic changes.
Nerve function.
Biomechanics (eg. leg length difference).
STRAINS
In most cases strains can be treated with osteopathy or physiotherapy using a variety of manual techniques and exercises. Sometimes even with mechanical back or neck pain, specialist assessment is necessary and investigations may be required.
SEVERE PAIN
Severe pain is assessed by our musculoskeletal physician, Dr John Tanner. Acute pain relief is provided by a variety of spinal injection techniques for conditions such as disc prolapse with sciatica or a trapped nerve in the neck.
CHRONIC MUSCULOSKELETAL PAIN
There are a variety of chronic pain relief techniques available at the Oving Clinic. These include utilising X-ray guided control to achieve targeted placement of medication and radio frequency thermal denervation. Fibroproliferative therapy to strengthen damaged or weakened ligaments is given as a course of treatment and followed with rehabilitation.
REHABILITATION
Rehabilitation programmes and home exercises are devised by our physiotherapists, and advice on preventative measures is given.
If you have further questions about this procedure please contact us.
Back to sport

It is essential for any sports person to minimise the impact of sports injuries on the ability to participate and complete. The importance of keeping people fit during the recovery process is vital. Cross-training, relative rest and support of injured structures make this possible.
Our team at The Oving Clinic offers an extensive range of treatments to achieve this. We have a wealth of experience within the sports injuries field. Some or all of the following services can be selected depending on the individual’s needs. We liaise closely with all parties: the sports person, coach, manager and GP
DIAGNOSIs
We provide early diagnosis in order to facilitate a speedy recovery; and full Sports Science back up for further analysis provided by colleagues in Sportswise Eastbourne or London.
TREATMENT
Treatment is carried out by Dr Tanner, who specialises in musculoskeletal and sports medicine, and our team of physiotherapists. This may include manual and assisted active mobilisation, injection techniques and electrotherapy.
PODIATRY
Where necessary, we offer podiatry involving assessment of gait, lower limb function, biomechanical analysis and design of
custom-made insoles.
REHABILITATION/PREVENTION
After the tissues have recovered enough to take the strain, we direct a graded return to pre-injury fitness through physiotherapy. A variety of techniques are used to mobilise and stabilise problem areas: these include manipulation, specific exercise, postural training and taping. Preventative measures such as adjustment of training programme, correction of faulty technique,advice on equipment and specific stretching and strengthening programmes are used.
OPTIMISING PERFORMANCE
This can be achieved by identifying musculoskeletal strengths and weaknesses; developing a personal programme; advice on nutrition; consultation with the coach; and full Sports Science back-up.
SPORTS AIDS
IS IT WORKING FOR YOU?
The most common reason for absenteeism from work is musculoskeletal pain. Our 12-point plan looks at how businesses can address this issue through analysis, ergonomics, treatment, fitness and stress management.
We have a wealth of experience in this area (British Gas, the Hampshire Police Force, Railtrack, IBM, Transco and South West Trains).
Our team of experienced and qualified practitioners offers an extensive selection of skills, treatments and therapies. This enables us to cross-refer and treat not only the physical aspects of the patient, but also the psychological and social.
Companies can choose some or all of the services in this programme. Patients are treated at our clinic or treatment rooms can be set up at the workplace either on a temporary or permanent basis. Qualified instructors can be provided to teach classes during the lunch hour or after work.
We liaise closely with all parties; the employee, the employer, physicians and other members of the Occupational Health Team including personnel and the employee’s GP.
12-POINT PLAN
1. Diagnosis of musculoskeletal problems with specialist back up.
2. Identifying any intrinsic or exrinsic factors that might influence the employee’s recovery.
3. Treatment for patients with particular or acute problems.
4. Low cost, high tech investigations and streamlined referrals to appropriate surgical specialists.
5. A pvhased return to work, or specific treatment that enables the employee to continue at work (i.e. with support and modified activities/work schedule).
6. Assessment of all/key employees for musculoskeletal risk factors.
7. Specific fitness programmes for high risk employees.
8. Advice on preventative measures and educating employees regarding their weaknesses in order to promote ‘self help’.
9. Advice on ergonomics (including statutory requirements).
10. Supply postural/musculoskeletal aids.
11. Stress management can be provided in light of the new legislation on stress-related disorders.
12. Preparation of medico-legal reports.
LIFELONG FITNESS

ASSESSMENT
A thorough assessment is given to clients wishing to embark on this programme which involves looking at areas such as cardiovascular and muscular endurance, strength, flexibility, speed, power, agility and coordination. A full medical history is also obtained.
PERSONAL PROGRAMMES
After analysing information gathered from the assessment, our team of physiotherapists will work with clients to devise a personal exercise programme.
NUTRITION
Nutrition plays an important part in the programme. A healthy, well balanced diet can help achieve fitness, a greater energy level, better complexion and positive attitude. We look at the individual’s eating habits and discuss how they could be improved.
RELAXATION
Allowing time for rest and relaxation is essential. We look at different methods of relaxation and help clients choose the most suitable one for them.
TRAINING
Once the individual training programme has been prepared, clients are encouraged to continue with the exercises at home or at the gym. Follow up appointments are held at the clinic after 6 weeks and programmes updated. For those who find it hard to exercise on their own, we can recommend a fully qualified personal trainer to visit the client’s home. Sessions may include jogging, step, aerobics, free weights, toning and stretching.
Spinal Health
Good posture, correct breathing, digestion and co-ordinated activity of upper and lower limb movements are vital for spinal health. In order to achieve these we need stability, flexibility, strength and control. If you are in pain, one or more of these components is affected.
DIAGNOSIS
This is the first step and a full assessment of all factors is essential.
These include:
Posture and movement patterns.
Joint mobility.
Muscle weakness or tension.
Ligament strain or slackening.
Degenerative or osteoarthritic changes.
Nerve function.
Biomechanics (eg. leg length difference).
STRAINS
In most cases strains can be treated with osteopathy or physiotherapy using a variety of manual techniques and exercises. Sometimes even with mechanical back or neck pain, specialist assessment is necessary and investigations may be required.
SEVERE PAIN
Severe pain is assessed by our musculoskeletal physician, Dr John Tanner. Acute pain relief is provided by a variety of spinal injection techniques for conditions such as disc prolapse with sciatica or a trapped nerve in the neck.
CHRONIC MUSCULOSKELETAL PAIN
There are a variety of chronic pain relief techniques available at the Oving Clinic. These include utilising X-ray guided control to achieve targeted placement of medication and radio frequency thermal denervation. Fibroproliferative therapy to strengthen damaged or weakened ligaments is given as a course of treatment and followed with rehabilitation.
REHABILITATION
Rehabilitation programmes and home exercises are devised by our physiotherapists, and advice on preventative measures is given.
If you have further questions about this procedure please contact us.